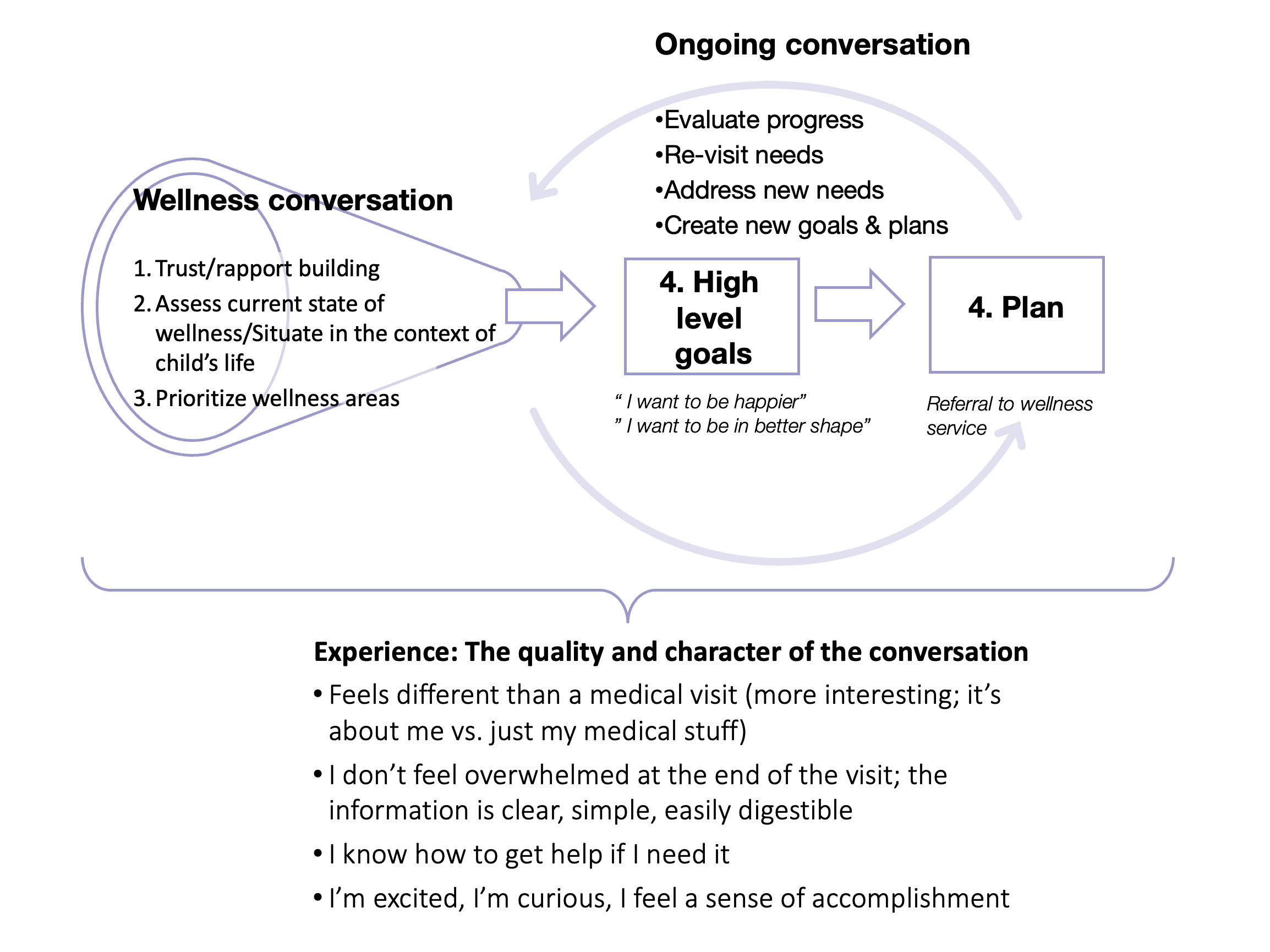
Through our work with patients and caregivers we have learned that the optimal way to connect patients with wellness services is to engage in a conversation that provides personalization and support. The schematic below represents a conversation that we designed using principles of the transtheoretical model of change, motivational interviewing, shared decision-making, and trauma informed care. We encourage you to mix and match tips from this curated set of resources to tailor wellness conversations to your patient's needs. For your convenience, here’s a link to our Provider Tip Sheet that we recommend downloading and using when making referrals to our program.
Also, if you're interested in learning more about the Wellness Center, explore our referral guidelines, the types of patients best suited for our services, and the holistic care we offer to support your patients’ well-being. Click here to watch a short medconnection video on how to refer and what to expect.
Referral Forms
New Patients (UCSF):
If you are a new patient and receive care at UCSF, please have your primary care provider or subspecialty care provider submit a referral through the online APEX medical record system.
New Patients (non-UCSF):
If you are a new patient and receive your care outside of UCSF, please have your primary care provider or subspecialty care provider download and complete our referral form.
Assess Readiness For Change
Top tips:
The stages of change, originated by James Prochaska, looks at how ready a patient is to embrace a new behavior. This can be used at various points in the wellness conversation to assess patient motivation for change either in a given wellness domain overall or around specific goal.
Stages:
-
Pre-contemplative
- As a provider you can help by focusing on building camaraderie and providing specific information.
- They may show lack of awareness, total resistance, or avoidance of a specific problem.
- Patients in this stage are unaware that a problem exists and have no plan for making changes.
-
Contemplative:
- Patients in this stage are aware there is a problem and are starting to think about how to approach it.
- They may still be weighing the pros and cons of changing or saying one thing but doing another.
- You can help by guiding the patient through evaluation of pros and cons and using the motivational interviewing and shared decision-making techniques noted below.
-
Preparation:
- Patients in this stage are ready to make change!
- They realize that change is needed, may share their plan for change with loved ones, and may even ask for help in making a plan.
- As a provider you can help them develop goals (such as personal vision/mission statements and "SMART" goals), guide them through small and achievable steps, and teach them skills they need to get there.
-
Action:
- Patients in this stage are taking action to make change.
- They might be asking for help, working on a plan, or actively changing their behaviors.
- As a provider you can help by assisting with resource identification, supporting patients as they troubleshoot their plans, and celebrating successes.
-
Maintenance:
- Patients in this stage have well engrained changes in their behaviors.
- They might embrance their new habits as part of an identity.
- As a provider you can help anticipate upcoming stressors and develop resilliency plans, help patients connect with long-term support systems, and celebrate longstanding achievements.
-
Recyling/Termination/Relapse:
- From time to time circumstances may lead a patient to fall out of their new habits.
- They might stop their new habit or start coping in a way that undermines their progress.
- As a provider you can help them process the new situation, assess when they are ready to re-engage in change, and help them to keep perspective.
Ready for more?
Get more background, specific examples of what to say, and tools to assess patient stage of change here:
https://www.aafp.org/afp/2000/0301/p1409.html
This flier from the Tennessee Alliance for Children and Families summaries the stages, along with indicators of each stage and provider strategies for each stage:
https://tnchildren.org/wp-content/uploads/2014/11/Stages-of-Change.pdf
Motivational Interviewing
Top tips:
This approach focuses on patient autonomy, embracing a spirit of collaboration between providers and patients and encouraging providers to evoke the patient's inner motivation for change. By empowering patients and their families, this approach can be used throughout the wellness conversation to ensure that we are honing in on the issues that matter the most to our patients and supporting them as they pursue their wellness journey.
What you can do: use the OARS method:
- ask Open-ended questions
- give Affirmations
- practice Reflective listening
- Summarize
Ready for more?
Review core skills in this summary article: Hall, Kate, Tania Gibbie, and Dan I. Lubman. "Motivational interviewing techniques: Facilitating behaviour change in the general practice setting." Australian family physician 41.9 (2012): 660-667. (https://www.researchgate.net/publication/230827341_Motivational_interviewing_techniques_Facilitating_behaviour_change_in_the_general_practice_setting)
Develop your confidence with this hour-long interactive session from BMJ learning: https://new-learning.bmj.com/course/10051582%20
Shared-Decision Making
Top Tips:
Shared decision-making is the formal process of collaborating with patients and families to ensure they understand their options and how those options align with their values and preferences. These skills will be integral to the wellness conversation as you select and hone goals.
Use the SHARE method:
- Seek your patient's participation
- Help your patient explore and compare options
- Assess your patient's values and preferences
- Reach a decision with your patient
- Evaluate your patient's decision
Ready for more?
Dive into details at the Dartmouth-Hitchcock Center for Shared Decision-Making: https://www.dartmouth-hitchcock.org/shared-decision-making/resources
The Agency for Healthcare Research and Quality has many resources for providers and patients:
https://www.ahrq.gov/health-literacy/professional-training/shared-decision/tools/index.html
Providing Trauma-Informed Care
Top tips:
Patients and families with pediatric onset chronic illnesses are repeatedly exposed to potentially traumatic medical situations. On top of this, they are more at risk for other childhood traumas, including adverse childhood events (ACEs) such as neglect and abuse.
The trauma-informed approach embraces key principles in the categories of: Safety; trustworthiness and transparency; peer support; collaboration and mutuality; empowerment, voice, and choice; and cultural, historical, and gender issues. We encourage providers to embrace a trauma-informed lens throughout the wellness conversation, specifically keeping in mind the 4Rs(below).
The 4 Rs
- Realization: Take the time to educate yourself about childhood traumas and their impact on childhood health.
- Recognize signs of trauma
- Respond: ensure that you a system that can respond to trauma
- Avoid Re-traumatization
If you are planning to screen patients for childhood traumas, we encourage you to work closely with a qualified social worker and/or mental health worker to minimize re-traumatization and ensure appropriate resources are available.
Ready for more?
Infographics and basics are available from the CDC: https://www.cdc.gov/cpr/infographics/6_principles_trauma_info.htm
SAMHSA has more indepth resources available here, including a complete guide to implementing trauma informed care at your clinic: